Back to: Paediatrics
Neonatal Conditions
Transient Tachypnoea of the New-born (TTN)
This is a condition which is the most common cause of respiratory distress in babies.
– In the fetus, the lungs are filled with fluid, however this normally gets squeezed out during vaginal birth and the remainder gets absorbed shortly after birth into the bloodstream.
– The problem arises when there is a delay in the reabsorption of lung fluid, which “drowns” lungs
– A risk factor is C-section delivery (as fluid is not squeezed out of the lungs)
Symptoms:
– Respiratory distress (tachypnoea, tachycardia, breathlessness)
Diagnosis:
– Diagnosis of exclusion once other more serious conditions have been ruled out
– CXR –> shows hyperinflated lungs with fluid in individual lung lobes
Management:
– Give oxygen to maintain O2 saturations
– Usually, it is a self-resolving condition as the fluid is absorbed into blood within days
Meconium Aspiration Syndrome
This is a condition which is caused by the foetus aspirating its meconium (first stool that the foetus passes)
– The meconium is a lung irritant and can lead to mechanical obstruction and chemical pneumonitis
Symptoms:
– Respiratory distress (tachypnoea, breathlessness, coughing) and hypoxia
– Risk factor for developing persistent pulmonary hypertension of the Newborn
– May also develop pneumonia and sepsis
Diagnosis:
– Can be diagnosed if you see baby with respiratory distress in infant born in dark meconium stained amnionic fluid
Management:
– Respiratory support (with mechanical ventilation) with anti-inflammatories/pulmonary dilators if pulmonary hypertension
Persistent Pulmonary Hypertension of the New-born (PPHN)
This is a condition which causes pulmonary hypertension in neonates.
– It is caused by failure of the pulmonary circulation to undergo the normal transition after birth
– There is sustained high pulmonary vascular resistance after birth which leads to pulmonary hypertension
– This can cause right-to-left shunting across persistent foetal shunts (PFO, PDA) and thus hypoxia
Causes:
– Primary –> idiopathic
– Secondary –> after birth asphyxia, meconium aspiration, sepsis
Symptoms:
– Gives cyanosis soon after birth
– Can lead to chronic lung disease leading to respiratory distress
– Increased incidence of hospital acquired infections
Test:
– Echocardiogram shows high pulmonary resistance
Management:
– Oxygen therapy (with mechanical ventilation) and pulmonary vasodilators to reduce resistance
Jaundice of the new-born
This refers to yellowing of the skin which occurs in 50% of all new-born infants
– It occurs as there is marked physiological release of Haemoglobin from RBC breakdown because of the high haemoglobin concentration at birth
– In addition, the RBC lifespan of neonates is shorter than that of adults (70d v 120d)
– Also, hepatic bilirubin metabolism is less efficient in the first few days of life
– It is also more common in breastfed-babies
Jaundice in the first 24 hours
Jaundice in the first 24 hours is always pathological. This is often due to conditions which release bilirubin into the blood. These conditions include:
– Haemolytic condition –> Hereditary spherocytosis and G6PD deficiency, ABO incompatibility
– Congenital infections –> rubella, CMW
– Haemolysis due to a haematoma
– Metabolic conditions –> Crigler-Najjar syndrome
The problem with neonatal jaundice is that is can lead to a condition known as Kernicterus:
– Unconjugated bilirubin is fat soluble so it can pass through the BBB
– It is neurotoxic, damaging the basal ganglia causing encephalopathy
Symptoms:
– Muscle hypertonia or hypotonia with spasm (torticollis)
– Opisthotonos –> hyperextension of back with extreme arching
– Inability to move the eyes up and down –> “sun setting” sign
– Seizures
– Lethargy and poor feeding
Diagnosis:
– Measure serum bilirubin level (blood test or transcutaneous bilirubinometer)
– The level is then plotted on a chart to see whether need to treat
Management:
Need for treatment and treatment options are determined using charts of the bilirubin level
– If below treatment line –> encourage feeds, avoid dehydration, and give support for breastfeeding
– If above treatment line –> 1st line is phototherapy (makes bilirubin water soluble to stop it crossing BBB)
–> 2nd line is exchange transfusion (removing baby’s blood and replace with donor)
Sudden infant death syndrome (SIDS)
This is the sudden unexplained death of a child <1-year-old, which occurs due to an unknown reason.
– It usually occurs during sleep, between the hours of midnight and 9am and is known as “cot-death”
– Whilst the exact cause is unknown, there are many risk factors which contribute to the syndrome
– In addition, certain factors like sharing the room with the baby and breastfeeding are known to be protective
Risk factors:
These are additive and together can give a much higher risk of death
– Infant –> Low birth weight, prematurity, male sex
– Parents –> Parental smoking, multiple births, maternal drug use, young mother <21 years old
– Environment –> Putting the baby to sleep prone (instead of on back)
– Bed sharing, infant pillow use
– Hyperthermia (over-wrapping) or head covering)
Diagnosis:
– It is a diagnosis of exclusion.
– Can only be diagnosed if the death remains unexplained after an autopsy, finding out the medical history of patient and family and investigation the death scene.
Management:
– After death, families are offering emotional support and grief counselling
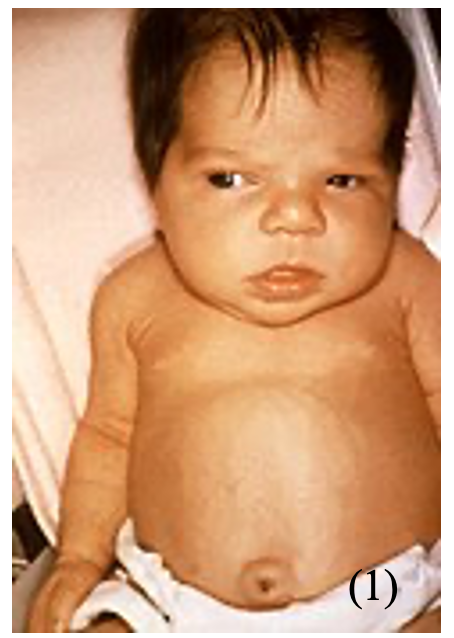
Congenital Diaphragmatic Hernia
This is a condition where the abdominal organs herniate a foramen in the diaphragm
– Most cases occur on the left-side and lead to compression of the lungs
– It occurs due to a failure of the pleuroperitoneal folds which form the diaphragm to seal, which leaves an opening through which the organs can pass through
– This allows the abdominal organs such as the bowel to pass through into the thorax

Symptoms:
– Pulmonary hypoplasia –> causes respiratory distress (SOB, cyanosis)
– Poor air entry into the left chest
– Raised blood pressure
– Apex beat and heart sounds displaced to right
Diagnosis:
– X-ray chest and abdomen shows loops of bowel in the chest:
Management:
– NG tube (suction of bowel contents) and intubation to secure airway
– Surgical correction is required
Hypoglycaemia
This refers to a low glucose level, generally considered as <2.6mM in the bloodstream
– A transient drop in blood glucose is commonly seen after birth as part of the adaptation to postnatal life
– Even term babies often get hypoglycaemic in the first 24 hours without any complications
– However, severe or prolonged hypoglycaemia may result in long-term neurological damage
Risk factors:
– Prematurity, infection, diabetic mothers, IUGR and macrosomia
Symptoms:
– Can be asymptomatic
– Can cause irritability, lethargy, apnoea, grunting, sweating, seizures
Management:
– If mild –> promote breast or bottle feeding
– If severe –> IV 10% dextrose
Haemorrhagic Disease of the new-born
This is a condition which causes bleeding in the neonate due to vitamin K deficiency.
– Vitamin K is needed as it is a cofactor for the carboxylation and maturation of various clotting factors
– It can lead to a spectrum of disease from minor bruising to large haemorrhages which can be seen up to 8 weeks after birth
Risk factors:
– Liver disease
– Maternal antiepileptic therapy –> these impair synthesis of vitamin K-dependent clotting factors
– Breast fed babies –> the breast milk is a poor source of Vitamin K
Symptoms:
These can occur up to 8 weeks after birth
– Bruising
– Haematemesis and melaena
– Potential intracranial haemorrhage
Management:
– IM Vitamin K and fresh frozen plasma if severe bleeding
Prevention:
– Vitamin K is offered all infants immediately after birth, usually as single IM injection
– Mothers on antiepileptics should receive oral prophylaxis from 36 weeks’ gestation
Sources
Image 1: Dr. Hudson, Public domain, via Wikimedia Commons
Image 2: © Nevit Dilmen, CC BY-SA 3.0 <https://creativecommons.org/licenses/by-sa/3.0>, via Wikimedia Commons


