Back to: Neurology
Nervous Systems
The PNS is divided into the somatic nervous system and the autonomic nervous system, which operates subconsciously, out of our control:
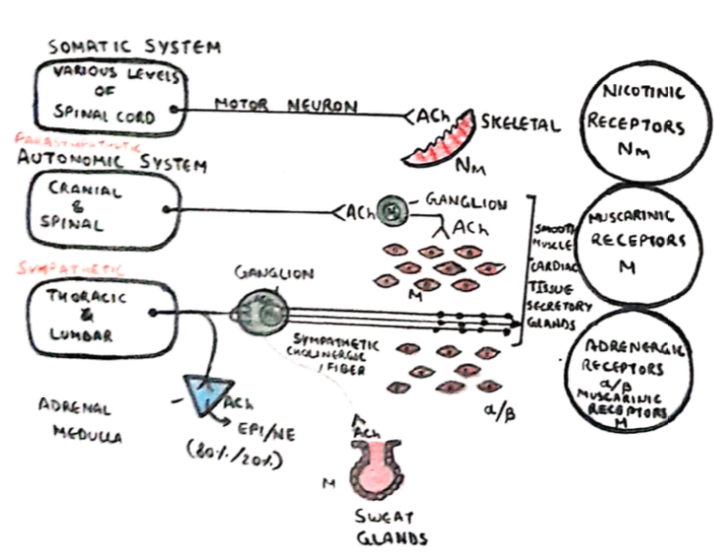
Somatic system
This controls skeletal muscle
– Motor neurons release ACh which acts at nicotinic ACh receptors
Parasympathetic:
– Preganglionic release ACh on nicotinic receptors
– Postganglionic release ACh on muscarinic receptors
Sympathetic:
– Preganglionic release ACh on nicotinic receptors
– Postganglionic release NA on adrenergic receptors.
ACh acts at the synaptic cleft and is broken down by phosphodiesterase enzymes into Acetyl CoA + choline
– NA is broken down by monoamine oxidase (MAO) and COMT into Vanylmandelic acid
Sensory System
This is composed of sensory receptors which transmit information to the cortex, in a series of levels.
Receptors
These are at the level of the skin and respond to specific modalities, activating sensory neurones
– The sensory neurones have cell bodies in the dorsal root ganglion, and then enter the spinal cord.
Spinal cord
Mechanosensation and proprioception travel in Aa and Ab fibres (large myelinated fibres.)
– These travel within the dorsal column of the spinal cord somatotopically (arm – lateral, legs – medial),
– They cross at the brainstem and ascend to the thalamus in the medial lemniscus
– Pain and thermoreceptors travel in spinothalamic tract in small unmyelinated Ad + C fibres
– These cross as soon as they enter spinal cord and travel in the contralateral, anterolateral system.
Somatosensory cortex
This is areas 1,2,3 and is responsive to somatic sensation.
– It is arranged somatotopically and represents the contralateral body.
Motor System
The motor system can be considered a hierarchy of information from the motor cortex to the effector muscles.
Motor Cortex
This is at the top of the hierarchy, which is anterior to the central sulcus
– Receives input from the premotor area which plans movements in response to external objects and Supplementary motor area (SMA) –> programs complex activity for voluntary movements
– The motor cortex has a map of the body: head- lateral, and legs- more medial, but the areas that require more control are over-represented.
– Lesions of M1give weakness rather than paralysis
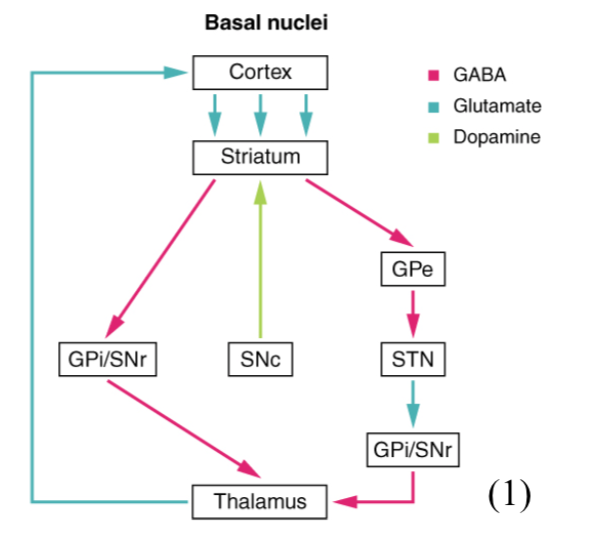
Basal Ganglia
This comprises of 5 nuclei.
– The signal from M1 is processed by the basal ganglia which decides if it is an appropriate movement – acting as a filter
– Inputs to the striatum are glutamergic excitatory. The rest are inhibitory.
– Direct pathway acts to disinhibit thalamus allowing more movements, whereas this is inhibited by the indirect pathway.
– Substantia nigra releases dopamine to increase transmission through direct pathway and reduce indirect pathway, disinhibiting thalamus
Cerebellum
This is required for learning movements and performing smooth intended movements.
– When learning new movements, long term depression occurs to over time increasing cerebellar output
The importance of the cerebellum is shown as lesions lead to ataxia, which is characterised by:
– Dysmetria (inappropriate displacement)
– Hypotonia (weakness)
– Dysdiachokinesis (inability to make rapid repetitive movements)
– Decomposition (lack of coordination of different joint movements)
Spinal cord
The main motor outflow tract is the corticospinal tract, through a-motor neurones
– Most fibres cross in the brainstem to supply contralateral muscles – travel in ventrolateral part of spine
– Lesions here (still UMN lesions) initially cause muscle weakness and loss of reflex
– They then give spasticity due to loss of descending regulation on sensory input and hyperreflexia.
Sources
1. OpenStax / CC BY (https://creativecommons.org/licenses/by/4.0)


