Anticoagulants
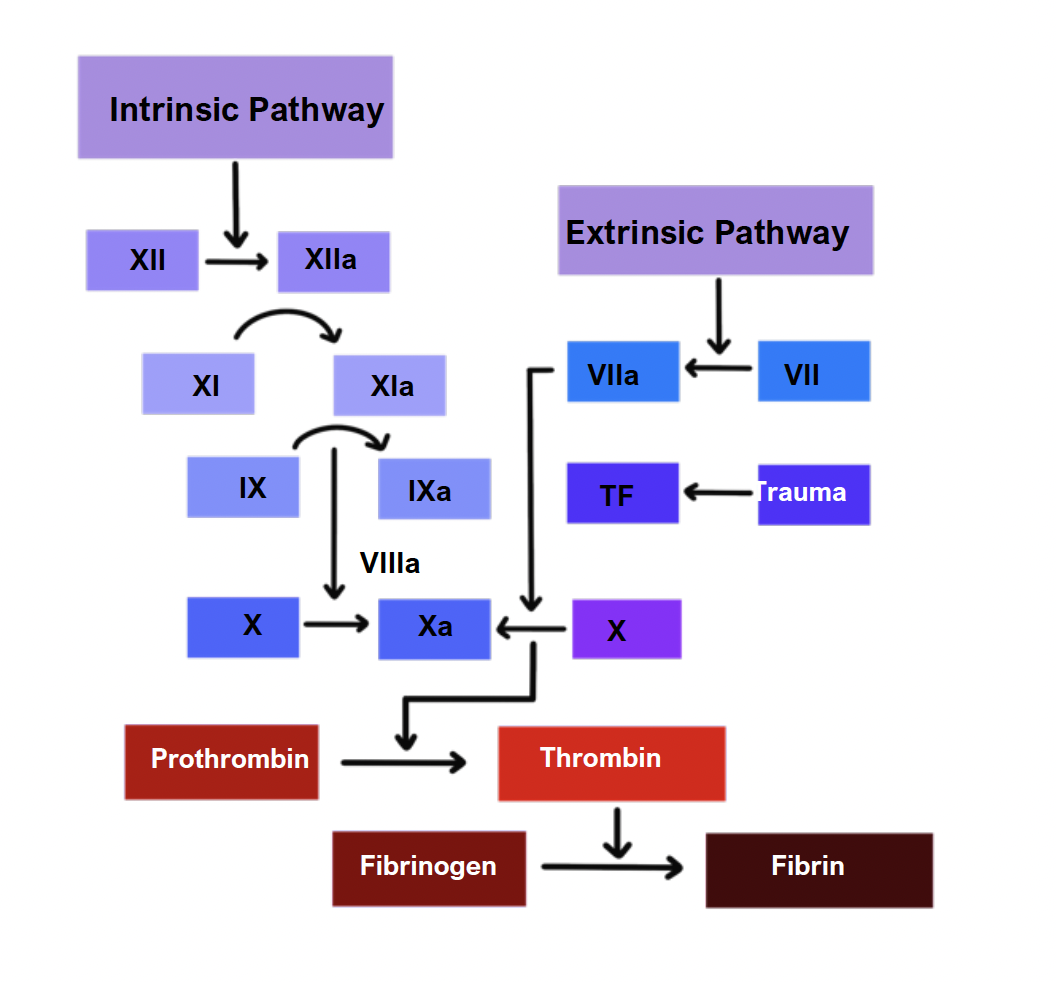
These drugs work by inhibiting specific aspects of the clotting cascade.
Heparin
Heparin is a natural anticoagulant produced by basophils and mast cells.
Heparins work by binding to and activating antithrombin-III (AT-III).
AT-III inactivates several clotting factors.
Different types of heparins are used therapeutically.
Unfractionated heparin
This is a type of heparin which has a short duration of action.
It binds AT-III, leading to inactivation of several clotting factors including II and X.
It is preferred for patients who have severe renal impairment and those who are at high risk of bleeding due to its shorter duration of action.
UFH is generally given as an IV infusion and monitored using APTT.
Protamine sulphate is used to reverse the effects of heparin.
Low molecular weight heparin – Dalteparin, enoxaparin
These have a longer duration of action.
They bind AT-III leading to more specific inactivation of factor X.
They are usually preferred because they carry a lower risk of heparin-induced thrombocytopaenia, and they are given by subcutaneous injection.
Fondaparinux
This is a drug which is chemically related to LMWH
Side effects
Common Side Effects:
- Haemorrhage –> manage by stopping drug and giving protamine sulphate to reverse the effects
- Heparin-induced thrombocytopaenia
- Skin reactions
Rare Side Effects:
- Osteoporosis
- Priapism
- Hyperkalaemia
- Alopecia
Contraindications
Should not be given to patients who are actively bleeding or high risk of haemorrhage
Warfarin
This is a drug which blocks the enzyme vitamin K epoxide reductase.
The enzyme is needed to produce the active form of vitamin K.
Less active vitamin K leads to reduced production of vitamin-K-dependent proteins.
This includes clotting factors II, VII, IX, X and factors C, S, Z.
It is given orally, has 100% bioavailability and a slower course of action than heparin.
Side effects
Bleeding – monitored by measuring the prothrombin time/INR
Skin necrosis and skin reactions
Blue toe syndrome
Metabolised by CYP450 enzyme – so affected by many other drugs and liver disease
Contraindications
Highly teratogenic so not used in pregnancy
However, it can be used while breastfeeding as significant levels are not found in breast milk
Novel oral anticoagulants
These are newer anticoagulants which directly inhibit certain clotting factors.
They are used in the treatment and prevention of venous thromboembolism and in the prevention of embolism in individuals with atrial fibrillation (in the absence of severe mitral stenosis).
These are newer anticoagulants which directly inhibit certain clotting factors.
They are used in treatment and prevention of venous thromboembolism and in the prevention of embolism in individuals with atrial fibrillation
Dabigatran
This is a direct inhibitor of thrombin.
It is reversed by the antidote idarucizumab.
Apixaban/Rivaroxaban
These are direct inhibitors of factor Xa.
Anti-platelet drugs
These drugs work to reduce the chances of thrombus formation by inhibiting the normal action of platelets interacting with the endothelium.
Aspirin
This is an acetylsalicylate which irreversibly acetylates and inhibits COX-1.
It decreases thromboxane A2 production in platelets which is a vasoconstrictor.
It also inhibits prostaglandin I2 production in the endothelium which is a vasodilator.
However, the endothelium can make new COX-1 whereas platelets cannot, which shifts the balance towards net vasodilation.
This inhibits platelet aggregation reducing the chance of clot formation.
It is used in patients with ischaemic heart disease and thrombotic stroke.
Side effects
Peptic ulcer formation
Reye’s syndrome – not given to children under the age of 16
Salicylism if taken in overdose
Dipyridamole
This inhibits uptake of adenosine and a PDE3 inhibitor which allows for vasodilation.
Ticlopidine, clopidogrel, prasugrel
These drugs inhibit platelet aggregation by inhibiting ADP from binding to the platelet P2Y receptor, which is usually responsible for platelet aggregation and stabilisation.
They are used in high-risk thromboembolism patients and coronary disease.
GPIIb/IIIa inhibitors
The GPIIb/IIIa is an integrin which allows fibrinogen-mediated platelet aggregation
Eptifibatide, tirofiban
These are inhibitors of the GPIIb/IIIa glycoprotein
Abciximab
A monoclonal antibody that binds glycoprotein to stop platelet aggregation
Thrombolytics
These drugs work to break down a clot once it has already formed, e.g., in stroke.
Fibrinolysis is achieved by producing the serine protease plasmin.
Inactive plasminogen is converted to plasmin by tissue plasminogen activators.
Fibrinolytics mimic activators to increase plasmin production to break down clots.
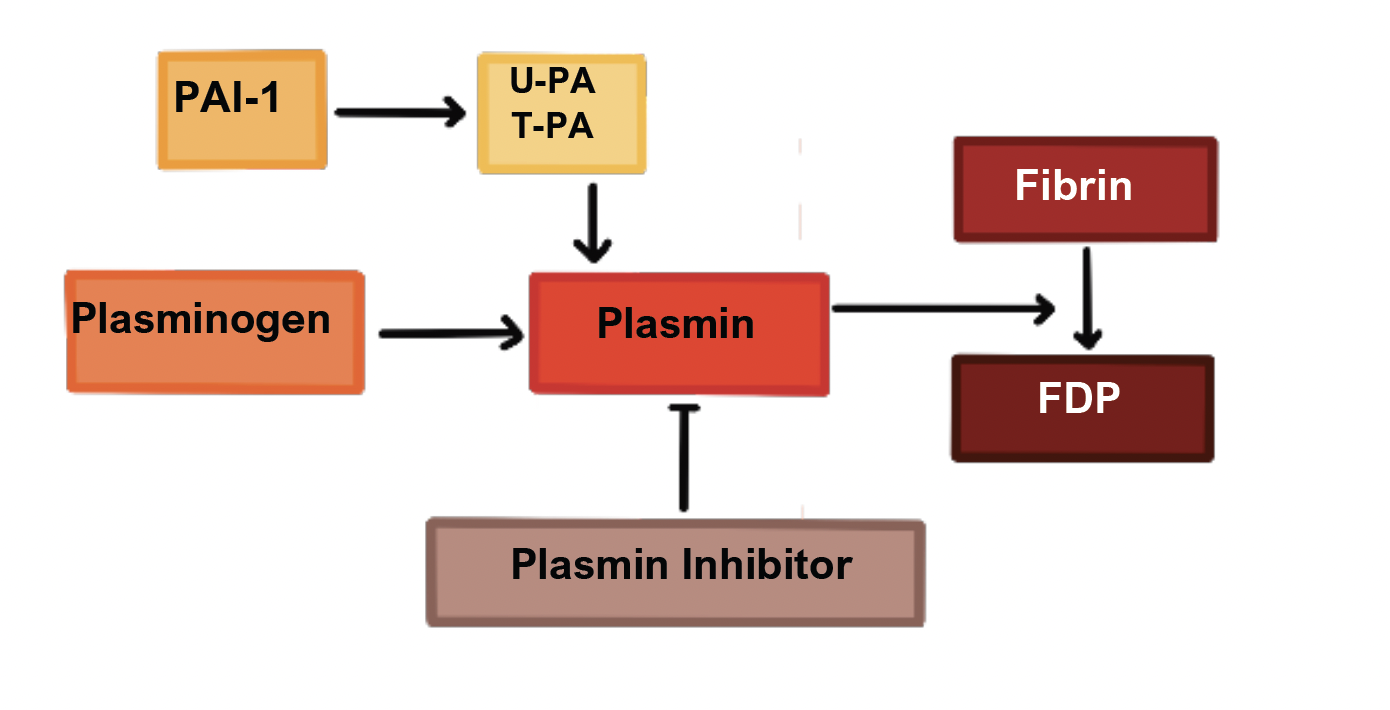
Streptokinase
This is an enzyme which is produced by streptococcus bacteria and binds to plasminogen to form plasmin.
Alteplase, duteplase
These are recombinant tissue plasminogen activators.
They are genetically engineered forms of human t-PA which have localised action on fibrin in clots.
Anistreplase
This is a combination of streptokinase and plasminogen.
It has a longer half-life than streptokinase and does not require circulating plasminogen.
Urokinase
This is a protease found in the urine which activates plasminogen.
It is used as an alternative in patients who are sensitive to streptokinase.
Side effects
Allergic reactions and anaphylaxis
Bleeding
Hypotension
Problems caused by reperfusion
Contraindications
Any condition which predisposes to bleeding is usually contraindicated:
| Bleeding |
|
| Trauma/ Surgery |
|
| Vascular |
|
| Cardiac |
|
| GI |
|
| Other |
|
Pro-thrombotic agents
These drugs may be used if the INR becomes too high, indicating a significant risk of bleeding.
They are also indicated in hypocoagulable states such as haemophilia and Vitamin K deficiency.
Vitamin K
This is required for the maturation of clotting factors II, VII, IX and X.
It is often given to newborns to reduce hypothrombinaemia in premature infants.
It is also used to reverse the effects of warfarin in patients.
Aminocaproic acid, tranexamic acid
These bind to plasminogen and prevent its conversion to the active form plasmin.
They are used to stop prevent/treat bleeding in trauma and conditions like menorrhagia and epistaxis.
Desmopressin acetate
This works by increasing synthesis of factor VIII
Therefore, is it issued to treat haemophilia A (deficiency in factor VIII)
Disclaimer