Antipsychotics
These drugs primarily work by blocking the dopamine D2 receptors in the mesolimbic and mesocortical areas of the brain.
The greater the dopamine receptor binding affinity, the better the clinical potency and efficacy of the drug.
They are classically divided into two major groups: 1st generation (typical antipsychotics) and 2nd generation (atypical).
Typical Antipsychotics
Haloperidol, chlorpromazine, fluphenazine, trifluoperazine
These drugs principally antagonise dopamine D2 receptors.
They give an immediate quietening action and have a greater effect on alleviating positive symptoms
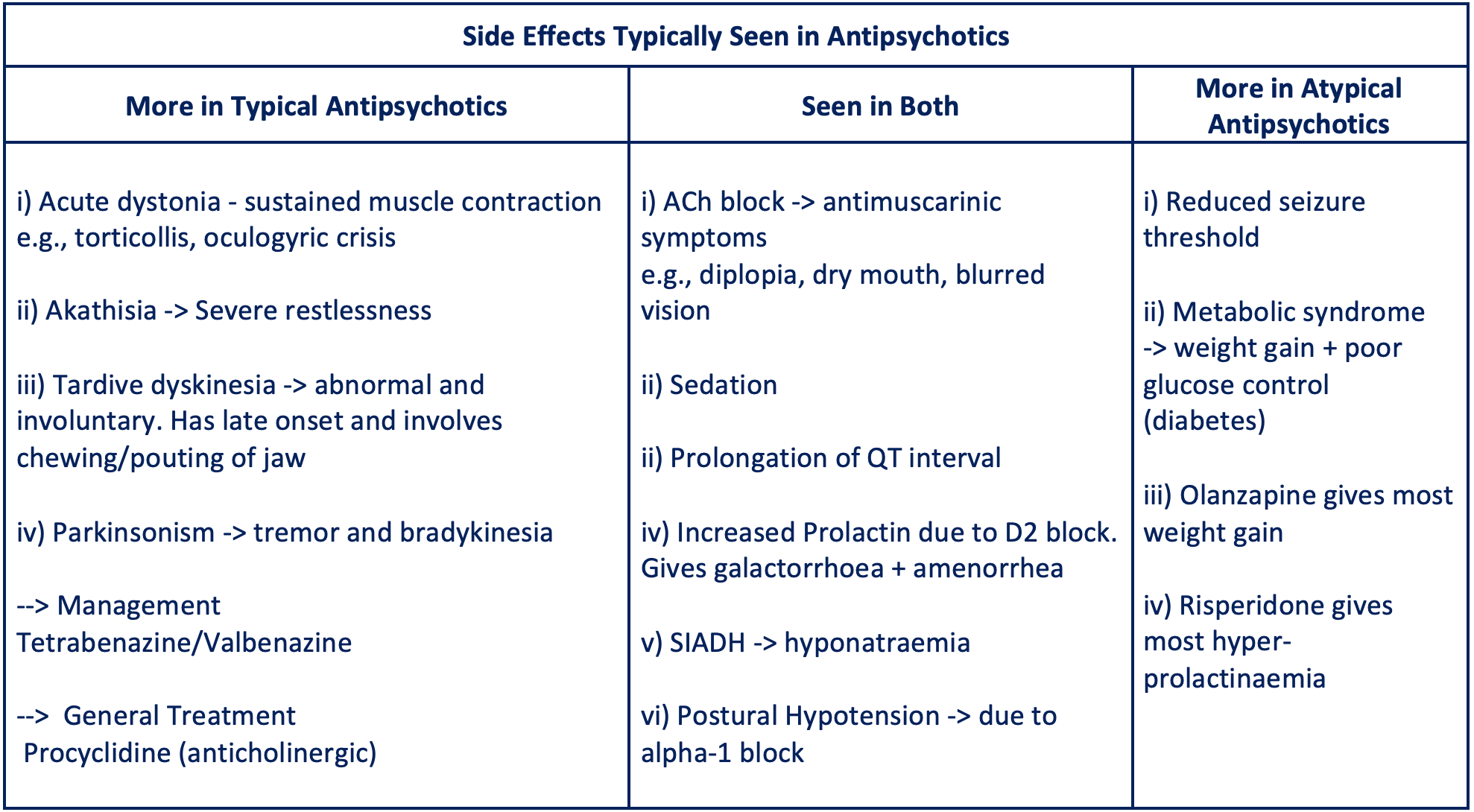
“Typical” refers to their propensity to cause extrapyramidal side effects, which are seen in greater incidence in this group compared to the atypical antipsychotic
Atypical Antipsychotics
Olanzapine, risperidone, quetiapine, aripiprazole
These drugs have lower D2 receptor affinity but also cause an additional block of 5-HT receptors.
They have an effect of alleviating both positive and negative symptoms.
These have replaced the typical drugs and are now first line for treatment.
They are less associated with causing EPSEs but have other effects.
Monitoring
As the anti-psychotics have so many side effects, regular monitoring FBC, U&E, LFT, blood glucose, BMI and prolactin is important.
These parameters are assessed on a variable schedule (e.g. baseline, at 3 months and then on an annual basis)
Also, as many affect the QTc interval, it is important to conduct a baseline ECG and carry out an annual cardiovascular risk assessment.
Aripiprazole
Unlike the other drugs, this is a dopaminergic partial agonist rather than antagonist.
It has the most tolerable side effect profile and is a good choice if patients have experienced or are at high risk of hyperprolactinaemia, metabolic syndrome or QTc prolongation.
Clozapine
This is a 3rd line treatment, only used in patients who are “treatment resistant”. It is defined as continuous symptoms after at least 2 trials of other antipsychotics.
It has a unique receptor profile acting on dopamine and serotonin receptors
It is very effective as an antipsychotic but has some serious adverse effects in addition to the ones above and complex prescribing involved.
Side Effects
Risk of agranulocytosis (neutropenia), particularly in the first year. This requires weekly FBC monitoring for the first 18 weeks.
Myocarditis and seizures – these are common on initiation.
CYP enzyme metabolism – the clozapine plasma level is increased when smokers stop smoking as smoking is a CYP enzyme inducer
Constipation, paralytic ileus and toxic megacolon
Hypersalivation
Neuroleptic Malignant Syndrome
This is one of the most dangerous complications of anti-psychotics
The dopamine blockade triggers massive amounts of glutamate release giving rise to sympathetic hyperactivity and muscle damage.
Risk factors include high doses of typical medications, rapid dose increases, underlying organic brain disease
Symptoms usually occur within hours to days of starting the antipsychotic.
Blood tests typically show an acute kidney injury, raised CK (muscle damage), leukocytosis (raised WCC) and a metabolic acidosis.
Symptoms
High fever
Muscle “lead pipe” rigidity
Low reflexes
Agitated delirium with confusion
Hypertension and tachycardia
Pupils are normal
Management
Stop the antipsychotic and treat the hyperthermia aggressively
May require supportive care in ICU with circulatory and ventilatory support
Dantrolene – this inhibits ryanodine receptors to stop Ca2+ release to relax muscle
Bromocriptine – this is a dopamine agonist which can also be used
Disclaimer